Learn About Tumor Immunotherapy
What is Tumor Immunotherapy?
Immunotherapy, also referred to as immune therapy, is a new approach for the treatment of cancer that harnesses the natural power of the immune system to combat cancer growth. The field of immune therapy is rapidly gaining recognition around the world for its potential to revolutionize cancer therapy. In fact, leading clinicians and scientists across the globe predict that it will soon stand alongside surgery, radiation and chemotherapy as the “fourth pillar” of cancer therapy – and that it may well prove to be the most important therapy of them all. We have already seen numerous success stories of cancers fought and lives extended through this treatment approach.
The immune system is our body’s specialized defense system against disease-causing germs, viruses and bacteria. Its primary function is to keep us healthy, and to combat illness and infections. While the immune system is effective against a whole host of invaders, it often lacks the intrinsic strength required to combat cancer on its own.
The goal of immune therapy is therefore to stimulate and enhance the disease-fighting responses of the immune system, such that they will be equipped with the necessary power and endurance to eliminate cancer from the body. One of the key players in this process is our white blood cells, and in particular, T cells. White blood cells are important cells in our immune system and can recognize and attack cancer cells. Immune therapy is based on the principle that if we properly stimulate the immune system, we will be able to use our own body’s system to treat cancer.
Immune therapy is particularly appealing because it can specifically target cancer tissues (and not healthy tissues) and thus generally has limited side effects. This is extremely exciting, considering the nature of chemotherapy and radiation therapy, which can damage healthy tissues in addition to cancerous tissues. In addition, immune therapy offers the chance of having a long-lasting effect for the patient, by taking advantage of the immune system’s remarkable ability to “remember” the invaders that it has eliminated in the past.
Immune Therapy Strategies
There are many steps that need to take place when the immune system is protecting the body from threats such as infections or cancer. We now know that the body also has different ways of potentially dampening the immune response, at each step of the way. Accordingly, there are a variety of strategies that can be used to enhance the immune response against cancer. These strategies can be grouped into the following categories:
- Immune checkpoint blockade
- Adoptive cell therapy
- Immune stimulation
- Cancer vaccines
Immune checkpoint blockade: There are various molecules that can dampen the immune response. In a healthy person, these ‘brakes’ or ‘stop signals’, act to hold the immune system at bay, preventing an over-activation of the immune response. Immune checkpoint blockade is based on using drugs that interfere with these brakes. This strategy, which blocks the stop signals, ends up unleashing the immune response, allowing it to destroy cancer cells. Recently, there have been major advances in developing these types of drugs. For example in the past few years, ipilimumab has been approved in Canada for the treatment of metastatic melanoma, and nivolumab and pembrolizumab, for the treatment of metastatic melanoma and non-small cell lung cancer. These drugs all target molecules that act as brakes on the immune response. Our team is investigating various aspects of immune checkpoint blockade, including basic biology that will lead to new therapies, and clinical trials of these agents and of combination therapies. Scientists have identified other such molecules and many pharmaceutical companies are developing new drugs that target them for cancer therapy.
Adoptive cell therapy: This type of therapy takes advantage of the cancer-fighting activity of a type of immune cell, called the “T cell”. In general, in adoptive cell therapy, a patient’s own T cells are taken into the laboratory, where their ability to destroy cancer cells is enhanced. These enhanced T cells are then given back to the patient. There are various ways to produce the enhanced T cells for therapy:
- T cells can be taken from within a tumor. These T cells are called “tumor-infiltrating lymphocytes” (TILs), and often have the ‘built-in’ ability to kill cancer cells. In the laboratory, TILs are activated and allowed to multiply, so that billions of cells can be transferred back into the patient, in the hopes of launching a stronger immune attack against the patient’s cancer. Our team is the only one in Canada currently testing this TIL-based immune therapy.
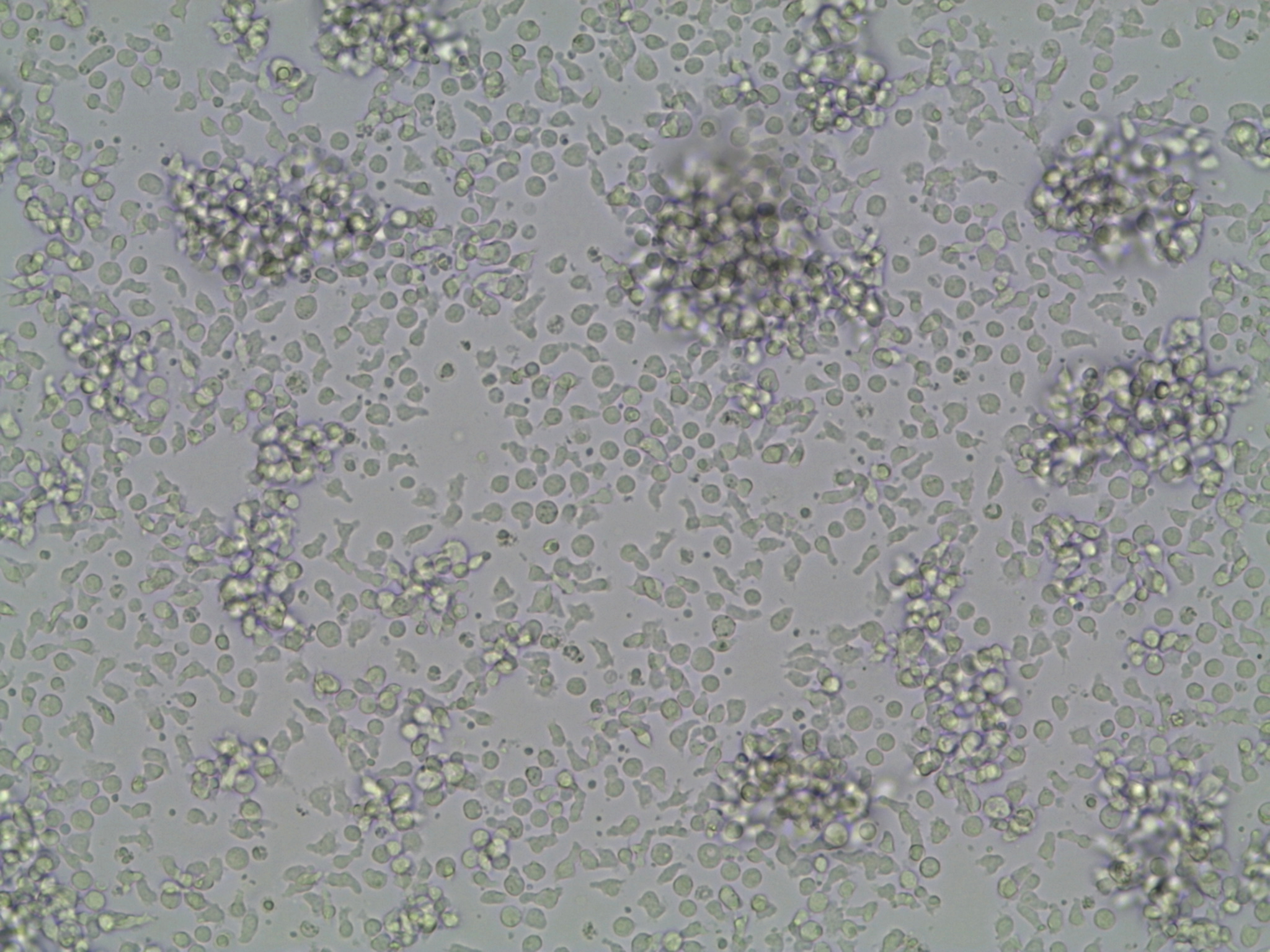 T cells being multiplied in the lab.
T cells being multiplied in the lab.
- T cells can also be taken from the blood, and then modified in various ways so that they can recognize and kill cancer cells.
- T cells can be modified so that they have a special protein called a T cell receptor (TCR) that can specifically recognize cancer cells. Our team is planning a clinical trial to evaluate this approach, called “TCR gene transfer”.
- Another special protein that allows T cells to recognize cancer cells is called a chimeric antigen receptor (CAR). When T cells are modified so that they have the CAR protein, not only can the T cells recognize cancer cells, they also gain particularly potent activity for killing the cancer cells.
- In another method, special tools can be used in the lab to selectively multiply T cells from the blood that are able to recognize cancer cells. Drs. Butler and Hirano have developed one such tool, called artificial antigen-presenting cells (aAPCs).
Immune stimulation: In the immune system, there are natural ‘accelerators’ or ‘gas pedals’ that can be activated to stimulate the immune system to attack cancer cells. In this strategy, drugs are used that take advantage of these ‘gas pedals’ and boost the immune response. Drugs that stimulate the growth of immune cells such as interleukin-2, or certain types of antibodies, can be administered to boost the ability of the immune response to attack cancer cells. For example, antibodies that stimulate proteins such as 4-1BB or OX40 are currently being tested as immune therapies, and many of these are being evaluated in ongoing clinical trials by our Drug Development Program.
Cancer vaccines: It is known that in the body, when the immune system encounters small pieces of cancer cells, it can potentially be stimulated to attack the cancer. The idea behind cancer vaccines is that if the right piece of a cancer cell is given to a patient, in the right format, then the patient’s immune system will launch a successful attack against the actual cancer cells in the patient’s body. Researchers have been studying what type of cancer vaccine has the best potential. The combination of cancer vaccines with other types of immune therapy, such as immune checkpoint blockade, may be a promising treatment for cancer.
Oncolytic viruses: Oncolytic viruses are unique because they can infect and destroy cancer cells, without harming healthy cells. Researchers now understand that oncolytic viruses can also activate the immune system against cancer. This two-pronged effect may represent a potent type of cancer therapy.
What is Immune Monitoring?
Immune monitoring provides insight into a patient’s own immune response over the course of a treatment. Information such as whether immune cells are functional or non-functional, and what specific proteins the immune cells can recognize on the cancer cell, can be essential in understanding if (and how) a treatment is working.
Personalized medicine is an emerging approach to health care in which medical decisions and treatments are tailored to the individual patient. Different properties of a patient’s cancer and their own immune system can have an enormous impact on a patient’s specific ability to mount a strong immune response against the cancer and to respond to a particular therapy. Understanding how different treatments impact the immune response against a patient’s own cancer is important for working towards improving cancer therapy.
In order to perform immune monitoring, blood or tumor tissue samples are taken from patients. Depending on the study, this can be done before, during or after the patient receives immune therapy (or at all three times). Through this immune profiling approach, we can test and define properties of the patient’s cells that correspond with successful or unsuccessful therapy. This information will help work towards:
- Uncovering ways to prevent and manage side effects of therapies.
- Discovering ways to know early during the course of treatment, whether a patient will go on to benefit from that treatment.
- Predicting which combinations of therapies have the best chance at success.
- Designing new therapies.
Our program has an Immune Monitoring Team that is dedicated to performing immune monitoring of patients receiving treatment for their cancer.
 [Insert caption]
[Insert caption]